Gut microbiome – Histamine Connection
Gut microbiome – Histamine Connection
Microvioma
May 16, 2024
Why Does This Matter to You?
Imagine eating a delicious meal and then experiencing unexplainable headaches, bloating, or a rash. You might blame it on stress or something you ate, but did you know that a little molecule called histamine, generated by bacteria in your gut, could be the cause? Lets explore the fascinating and intricate relationship between your gut microbiota and histamine, explaining why this connection is critical to your overall well-being.
Understanding Histamine.
Histamine is a naturally occurring chemical that plays important roles in your immune, digestive, and central neurological systems. It is well-known for its role in allergic reactions, which include symptoms such as itching, sneezing, and watery eyes. Histamine’s influence, however, goes beyond allergies and has a significant impact on gut health.
Your gut microbiome is a vast, dynamic ecosystem made up of billions of species, including bacteria, viruses, and fungi. These microorganisms are crucial for a variety of biological activities, including food digestion, vitamin synthesis, and immune system regulation. Importantly, certain bacteria in your gut can create histamine, which affects your health in a variety of ways.
Histamine and Gut Microbiome: The Connection
Histamine-producing Bacteria
Certain bacteria in the gut, including those from the genera Enterobacter and Lactobacillus, can create histamine by decarboxylating the amino acid histidine. While this is a natural aspect of microbial metabolism, an imbalance or overgrowth of these bacteria might result in excessive histamine release.
Histamine Degradation and Enzyme Deficiency
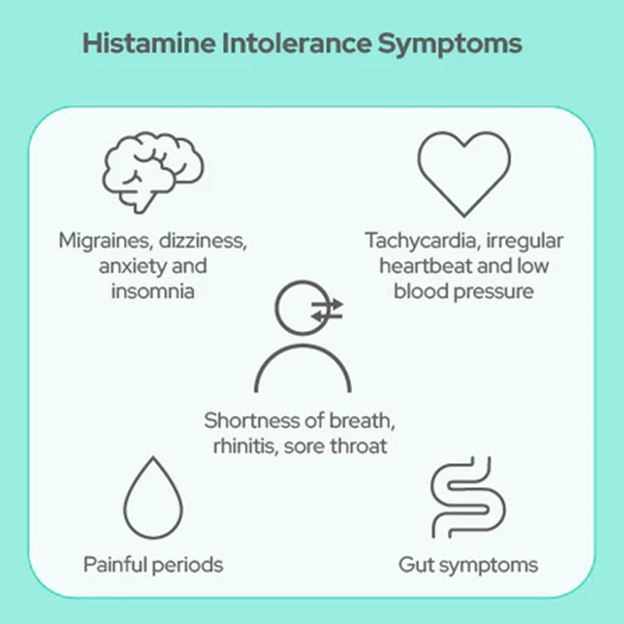
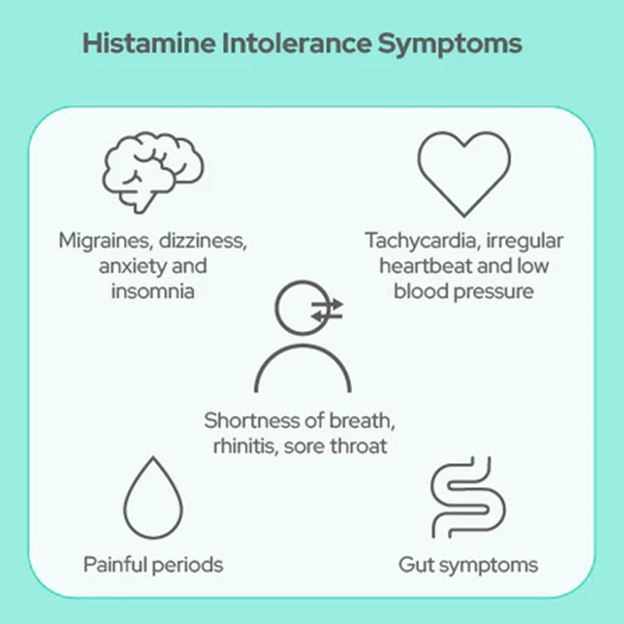
Normally, enzymes like diamine oxidase (DAO) and histamine N-methyltransferase (HNMT) break down histamine to keep it in check. However, if these enzymes are defective or inhibited—due to genetic factors, some drugs, or gut health issues—histamine levels might rise, causing a variety of symptoms. The condition also known as histamine intolerance (HIT), can cause headaches, gastrointestinal discomfort, skin rashes, and more.
Dysbiosis of the microbiome and histamine intolerance
Dysbiosis, or an imbalance in the gut flora, can worsen histamine-related symptoms. For example, a reduction in helpful bacteria such as Bifidobacterium and Faecalibacterium prausnitzii might disturb gut health, allowing histamine-producing bacteria to thrive. This imbalance not only raises histamine levels, but also limits the body’s capacity to breakdown it, exacerbating symptoms of histamine intolerance.
Real-Life Implications
Food Allergies
Histamine has an important function in food allergies. When the immune system incorrectly recognizes some dietary proteins as dangerous, it causes an allergic reaction by releasing histamine from mast cells and basophils. Elevated histamine levels can cause symptoms ranging from minor discomfort to serious, life-threatening reactions such as anaphylaxis. Studies have revealed that using H2 receptor antagonists in people might boost IgE synthesis against food antigens, linking histamine to allergic reactions.
Irritable Bowel Disease (IBD)
Mutations in histamine receptor expression and elevated mucosal histamine levels are common in diseases like Crohn’s disease and ulcerative colitis. These modifications exacerbate inflammation and the severity of the illness. The way histamine regulates cytokines like TNF-α and IFN-γ highlights how important it is for the development of IBD. IBD patients may benefit from regulating histamine receptor activation, according to research.
Inflammatory Bowel Disease (IBS)
Histamine levels in the gut are frequently higher in IBS patients, and this is correlated with the severity of their symptoms. IBS symptoms can be made worse by dysbiosis, which is defined by an overabundance of bacteria that secrete histamine. Higher amounts of histamine have been found in supernatants from colonic samples of IBS patients, suggesting a direct correlation between gut microbiota and histamine in this illness.
Controlling Histamine Amounts
Considering the negative effects of histamine on health, controlling histamine levels is essential, especially for people who have histamine intolerance or other gut diseases. Here are a few doable actions:
- A diet low in histamines may aid in symptom reduction. This entails staying away from foods high in histamine, like some fish, old cheeses, and fermented goods. In general, fresh, unprocessed meals are safer.
- DAO supplements can help patients with enzyme deficits by aiding in the breakdown of dietary histamine.
- Bifidobacterium strains in particular are known to help balance the gut microbiome and lower histamine production. Early studies indicate that probiotics may be a promising adjuvant therapy, but additional research is required.
The intricate connection between your gut microbiome and histamine is a vital aspect of the overall health. Gaining insight into this link can enhance your quality of life and assist in managing ailments including food allergies, IBD, and IBS. You can control your histamine levels and keep your gut healthy by following a well-informed diet and maybe taking supplements. We will learn more about this intriguing interaction and its consequences for wellness and health as study advances.
READ FURTHER :
Histamine: A Bacterial Signal Molecule: https://tinyurl.com/tbzfdh6j
Histamine Intolerance—The More We Know the Less We Know. A Review: https://tinyurl.com/2vab8cay
Histamine Intolerance Originates in the Gut: https://tinyurl.com/bdcpmza8